Neck Pain More Common Than Nausea in Migraine
Emma Hitt, PhD
In patients with migraine, neck pain was more commonly associated with migraine than was nausea, which is considered a defining characteristic of the disorder, a new study shows.
“The finding that neck pain was more commonly associated with migraine than was nausea would seem to be a big surprise, given the absence of its mention in textbooks and in The International Headache Classification II (ICHD-2) criteria,” said lead author Anne H. Calhoun, MD, with the Carolina Headache Institute in Chapel Hill, North Carolina.
“However, when we first presented these findings at the American Academy of Neurology meeting, the response from headache specialists was almost universal: vigorous nodding and assent,” she told Medscape Neurology. “This is something that many experienced headache specialists have noticed but have never reported.”
Their report was published online January 20 in the journal Headache.
Clarify Migraine Diagnosis
The prospective study included 113 patients with migraines, who had a frequency of attacks from episodic to chronic migraine and who were followed up for at least 1 month and until 6 migraine episodes had been treated.
Patients were also assessed for headache intensity, the presence of nausea, and neck pain. Data on 2411 headache-days were collected, including 786 days on which patients had migraines.
“Regardless of the intensity of headache pain at time of treatment, neck pain was a more frequent accompaniment of migraine than was nausea (P < .0001),” note the study authors. “Prevalence of neck pain correlated with chronicity of headache as attacks moved from episodic to chronic daily headache.”
According to Dr. Calhoun, many clinicians associate the presence of neck pain with a tension-type headache, “relegating many patients incorrectly to treatment with muscle relaxers, tranquilizers, or various OTC [over-the-counter] analgesics.”
“We hope that this paper will clarify migraine diagnosis for primary care physicians who are charged with staying current with scores of diverse medical conditions and their diagnostic criteria,” she added. “Ideally, these findings will ultimately be confirmed and incorporated into ICHD criteria.”
An unanswered question, said Dr. Calhoun, is the issue of underlying pathophysiology. “The neck pain may be a sign of central sensitization and/or a marker for chronification in migraine (as the headache disorder moves from episodic to chronic daily headache), but this remains to be proved.”
Findings Useful
Randolph W. Evans, MD, with the Baylor College of Medicine in Houston, Texas, noted that these findings probably reiterate previous findings but may be useful in helping to distinguish migraine from other types of headaches.
“About half the people who have migraine don’t realize that they have migraine,” Dr. Evans told Medscape Neurology, “so the findings are useful in helping to differentiate migraine from a simple tension-type headache and to understand how commonly migraines can cause neck pain as part of the migraine attack.”
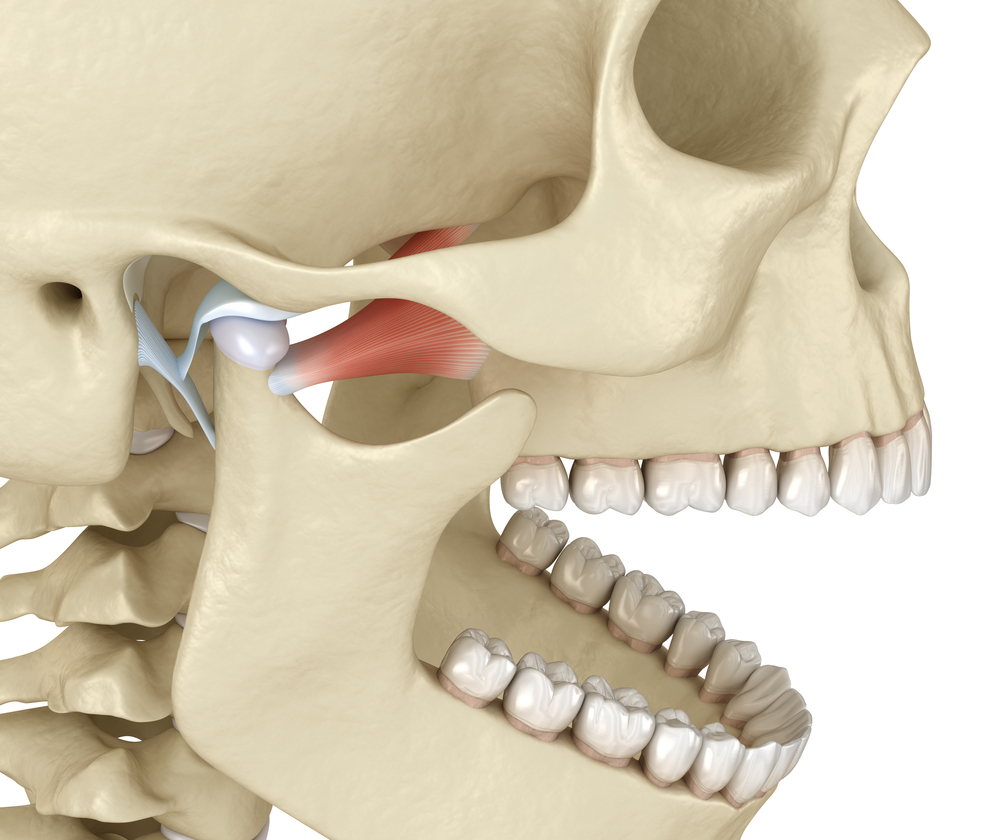
Till Sprenger, MD, from the University of California, San Francisco, pointed out that the trigeminal second-order neurons in the trigeminocervical complex receive convergent input from trigeminal and C1 and C2 innervated areas that can lead to referred pain and, moreover, that these neurons can be sensitized during migrainous pain.
Because of this, Dr. Sprenger agreed with Dr. Calhoun and Dr. Evans that these findings are not a real surprise for clinicians experienced in the headache field, but noted that it is useful to have a properly conducted trial confirming that neck pain is an integral symptom of migraine.
“Many headache patients have imaging studies of their neck, typically MRI [magnetic resonance imaging], before they are seen by a headache specialist, and most, almost all, of these imaging studies are unnecessary,” Dr. Sprenger said.
This investigator-initiated study was funded by GlaxoSmithKline. Dr. Calhoun receives research support and is a consultant for Teva Pharmaceuticals. Dr. Evans has disclosed that he has served as an adviser or consultant to Merck, Ortho-McNeil, Pfizer, and GlaxoSmithKline.
Headache. 2010;67:154-160.
Dr. Stan Farrell is Board Certified in Orofacial Pain and has extensive training in the treatment of migraine headaches. As indicated in this study, you may experience referred migrainous pain through the trigeminal nucleus caudalis. Various known headache triggers can cause migrainous pain to travel to different areas of the head and neck. This is how TMJ, a known headache trigger, can cause migraine headaches or neck pain. If you are experiencing migraine headaches, call and schedule a consultation at AZ TMJ, 480-945-3629.